Authors: Doug Franzen, MD, Linda Katirji, MD Michelino Mancini, DO, Lesley Walinchus-Foster, MD, Meredith Wittie, MD, Alexis Pelletier-Bui, MD and Caitlin Schrepel, MD on behalf of the CORD-Advising Students Committee in Emergency Medicine (ASC-EM)
This applying guide is intended for students who are interested in applying to Emergency Medicine (EM) residency programs, but do not have direct access to an adviser that is a faculty member at an EM residency program (hereafter referred to as “orphan” applicants). This guide is intended as a supplement to the General EM Applying Guide.
The application and match process in EM have undergone significant changes in the past few years. This guide is meant to provide further detail to students who do not have an EM residency faculty member familiar with recent changes to help guide them through the application process. If you have access to an adviser who is currently a faculty member at an EM residency program, we highly recommend that you go to that individual for guidance. This written guide provides a broad overview of the application process in EM and is not meant as a replacement for individualized advising.
This guide is meant for final year medical students (both MD and DO) in the United States, entering the match for the first time. We recognize that students outside the United States have the same problem (lack of an EM adviser) but International Medical Graduates (IMG’s) face additional hurdles and an entire guide has been written for that population: the IMG Applying Guide. If you have already graduated and are going through the Match a second time, see the Re-Applicant Applying Guide.
Based on the locations and affiliations of existing residency programs, orphan applicants are more likely to be Osteopathic students. If you are an Osteopathic student, we strongly recommend reading the Osteopathic Applying Guide in addition to this guide. Additionally, orphan applicants may have other issues such as Couples Matching or Military Matching. If so, you are advised to review those guides in addition to this one.
Finally, this guide discusses things that will occur over the course of a year or longer. We advise that you review it all once to get an overview, and then return to each section as you move through the process.
Overview of the Match Process
As you may know, the third Friday of March is Match Day – the day when medical students learn where they will be doing their residency. The process leading up to the EM match starts almost a year before. Students applying in EM are strongly encouraged to complete two EM rotations, at two different institutions (see “Away Rotations” below). Your performance on each EM rotation is used to generate a SLOE (Standardized Letter of Evaluation), a key part of applying in EM. At least one SLOE needs to be in your file prior to submitting your application in EM – according to EMRA Match, fewer than 5% of programs will accept your application without one. Most students complete their first EM rotation between about April and August, with their second rotation completed by October. Arranging rotations can take some time, so many students start looking for rotations in about March – i.e. a year before their Match Day. One other unique element to applying in EM is the Standardized Video Interview (SVI). This needs to be completed between June 7 and July 15. In addition to these unique elements, you still need to do the things students matching into other specialties are doing: write a personal statement; request general letters of recommendation; meet with your dean to review your Dean’s Letter (MSPE); fill out an Electronic Resident Application Service (ERAS) application; and decide to which programs you’ll apply.
If you are more than one year away from matching, one of your first priorities should be gaining experience in EM to ensure it’s the right career choice for you. You can also consider some of the following steps to make yourself a more competitive applicant in EM. (See the Orphan Student Planner on the CORD ASC-EM webpage and this page for more information.) In addition to doing well in your classes, things to consider include: joining your school’s EM interest group (EMIG) – or starting one, if your school doesn’t have one; joining and becoming active in the Emergency Medicine Residents’ Association (EMRA); going to state, regional, or national EM conferences (American College of Emergency Physicians (ACEP), American Academy of Emergency Medicine (AAEM), or the Society for Academic Emergency Medicine (SAEM)); completing a research project (this doesn’t have to be done with an Emergency Physician – you can find projects that are relevant to EM in just about any specialty); and volunteering.
As noted above, a successful match will require planning in order to complete the USMLE exams and schedule two EM rotations early in the fourth year, so that you have SLOEs submitted ERAS in time to submit your application. In addition to having all of the required elements, it is also important to avoid any “red flags” on your application that would diminish your chances of matching. These include: failing classes/rotations, failing or scoring low on USMLE examinations, felonies, professionalism issues, and unexplained gaps in training. Although they do not necessarily mean you won’t match in EM, if you do have any of these “red flags,” the process will be much more difficult for you. Refer to the At-risk Applicant Applying Guide for additional information and ways to address these issues.
Advising and Advisers
If possible try to find a mentor or adviser. If you are reading this, you are considered an “orphan” applicant, meaning that your school isn’t affiliated with a training program or lacks EM faculty that can advise EM-bound students. A good mentor can be critical to helping you through the process. Try to find an EM faculty adviser who is involved with an accredited EM residency program. These faculty are the most familiar with the application process and will be able to give the highest quality advice. The application process in EM has gone through some big changes in the past few years and continues to evolve. An adviser who is affiliated with a residency program will be aware of these changes and can help ensure your application has everything you need. Residency affiliated faculty can also help you with questions such as how many or which programs to apply to. While deans and other non-EM faculty may offer great advice on the application process in general, they may not be fully aware of how applying in EM is different from other specialties. Local Emergency Physicians who went through the match process more than a few years ago can provide some good insight about careers in EM, but won’t be aware of the most recent changes in the Match process.
If your school has one, you may be able to locate a mentor through the Emergency Medicine Interest Group (EMIG). The EMRA Medical Student Council is another source that can help you locate a mentor. Students can also participate in large-group virtual advising sessions through EMRA Hangouts – real-time, online question and answer sessions. The EMRA Hangouts site also has an archive of prior sessions you can watch. Other options for EM application and career guidance include:
1. Attend a regional or national EM conference; many have advising forums and/or the opportunity to network with program faculty. ACEP in the fall and SAEM in the spring both offer residency fairs.
2. Look for fellow students who are interested in EM, or prior graduates of your school who matched in EM. Your dean’s office can help in this task. Ask upperclassmen how/when/where they found a mentor. Query their personal experiences and listen to their recommendations. Someone who has just completed the process can have invaluable information.
3. Reach out to a program you’re interested in to see if they have faculty that will advise you. Faculty mentors are often available during your out-of-town rotations; consider asking one of their residency leaders for advice or help locating an adviser.
In addition to finding a mentor who is affiliated with an EM residency program, we strongly recommend that you join EMRA and investigate SAEM and other professional organizations.
Additional advising resources from CORD ASC-EM and EMRA can be found here and here, respectively.
Letters of Recommendation
EM utilizes a unique, standardized letter as part of their application process, the SLOE. Here is an example of what the SLOE looks like. The first page is about your performance as a student in the Emergency Department; the second page focuses on how you might perform as an EM resident. Surveys of EM program directors show that the SLOE is one of the most important parts of an applicant’s file. Although letters of recommendation from other rotations are often submitted, these are not given the same weight as letters from EM rotations. (See also “The Hierarchy of Letters” in the General Applying Guide)
The letters of recommendation that carry the most weight come from residency program leadership, and in the last few years the trend has been towards “group SLOEs” written by the educational teams where you rotate (often including both the program director and clerkship director, as well as other core faculty members). These letters carry more weight than traditional letters of recommendation because they provide context for direct comparison of you to your EM-bound peers by people integral to the EM match process. You should aim to get two SLOEs from academic residencies.
While community EM months can be great learning experiences and expose you to how the majority of EM physicians practice, they will not significantly assist your application to an Accreditation Council for Graduate Medical Education (ACGME) EM residency. A letter of recommendation, or even a SLOE written by a doctor at a community ED is not the same as one from an ACGME program and may not be counted as equivalent. If your school requires a community EM experience, you will have to do extra clerkships in EM, and in some instances even forgo credit to gain the right experience to help your application.
More information about Away Rotations can be found below.
Board Scores
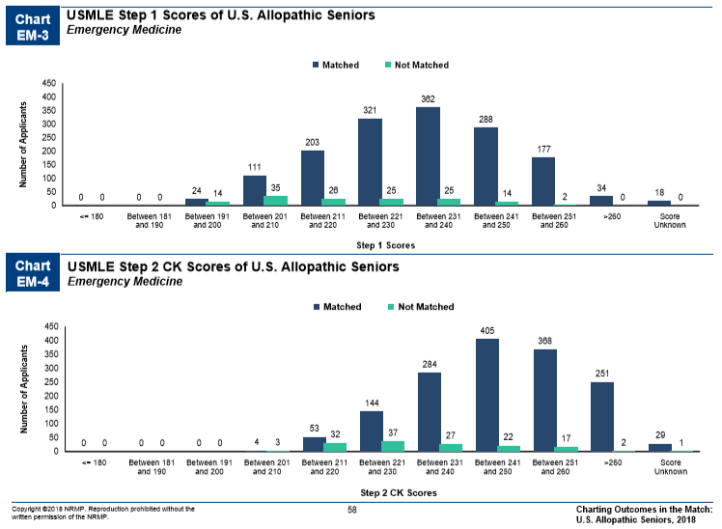
As in other specialties, USMLE scores are an important consideration for applicants to EM Residency Programs. The mean USMLE Step 1 and Step 2 CK scores for US allopathic medical students who listed EM at the top of their rank list and successfully matched into EM in 2018 was 233 and 247 respectively (see figure 1 below). Scores below 220 may make it much more difficult for you to get interviews and hence match into EM. For USMLE Step 1 scores <220, you may want to consider a backup plan – this is something that should be discussed with an adviser familiar with advising EM applicants. If your Step 1 Score is <220, try to take USMLE Step 2 early in your fourth year so that you can have your scores available when ERAS opens and no later than October 1st.
Away Rotations
Fourth year EM clerkships are the first foray into the ED for most applicants. As a student without a home residency program, you are in a unique position when compared to others who have a “home” program in EM. In addition to picking up the basics of EM, away rotations afford you the opportunity to connect with mentors at established academic institutions, be exposed to working with residents, participate in resident conferences, and share application strategies with other students. Clerkship directors or a faculty mentor assigned or acquired on shift can help guide you through the application process or serve as an adviser. S/he can be a good source of advice about programs in the local area, your competitiveness as a student, and which programs you might want to consider when applying.
How Many Rotations Should You Do?
The recommendation is TWO rotations in EM (i.e. TWO rotations at EM residency training programs that can provide SLOEs). You may hear of students doing more than two EM rotations. This is recommended in some circumstances, such as couples matching, but is generally not necessary for most applicants. Use your fourth year to explore other aspects of medicine! Become an expert at slit lamps or differentiating rashes. For most students, this means doing a rotation at their home rotation, and a second rotation at another institution (the thought behind this is that a letter from the visiting rotation will be less biased). As an orphan, you will need to complete two visiting rotations. These rotations should be done as early as possible in order to secure a first SLOE prior to submitting your application, and a second SLOE before interviews. Ideally, both SLOEs are submitted with your application on September 15th but this is not always possible. You will need to submit at least one SLOE with your initial application; the second SLOE can come a little later. Although all clerkship directors are well aware that the SLOE is a requirement for EM applicants, it is good to let them know that you would like a SLOE from the rotation. Many clerkship directors will ask you for your personal statement and CV at the beginning of your rotation to help them write the SLOE. Although your personal statement might not be a masterpiece at this time, clerkship directors and program directors use this to get to know you better — so even if it’s still in draft form, don’t be afraid to share it. Many clerkship directors are happy to help you revise your personal statement.
Which Types of Programs Should I Apply To for an Away Rotation?
A SLOE carries the most weight when written by a consensus panel or faculty member from a large academic center that is affiliated with a residency program. As an orphan applicant, it is especially important that your SLOEs come from a residency program, as the main goal of the SLOE is to evaluate how you will perform as a resident. We recommend that you rotate at the residency’s main site. Investigate thoroughly, as some programs offer rotations at smaller affiliate sites and a SLOE from such a site will not carry the same weight as one from the main site. Additionally, many sites offer “EM Electives” such as toxicology, ultrasound, Pediatric EM, Wilderness Medicine, and others. While these rotations can be a great way to learn more about a program, SLOEs from these elective rotations are not given the same weight as those from true ED rotations.
Other things to consider when applying to away rotations are geographic location, patient population, length of program (3 or 4 years) or academic versus community centered programs. Ideally, your visiting rotation is at a program where you would like to complete your residency training. However, that can be hard to know this early in the process. If you are unsure of where you want to train in the future, an away rotation in both an urban and more rural location can help you decide.
How Do I Find Away Rotations?
Visiting Student Learning Opportunities (VSLO, formerly VSAS)
Much like residency applications, away rotations have a system for standardized applications. VSLO is a centralized application system used by many (but not all) clerkships. Your dean’s office may be familiar with VSLO as it is used in many specialties, not just EM. If you are not familiar with VSLO, there is a FAQ list on the website. CORD ASC-EM has also posted some basic tips regarding VSAS/VSLO. The VSLO database will provide you with the starting dates of rotations and requirements for each institution. Pay particular attention to the required documentation for each institution. Get those taken care of ahead of time – know which immunizations, forms of identification, testing requirements, miscellaneous documents you need so you don’t miss out on a rotation!
Non-VSLO/VSAS institutions
There are several institutions that do not participate in VSLO. The EMRA Match tool now includes clerkships (click “more filters” and scroll down to “Student Rotations”) and can easily identify which programs will ask for a separate application for an away rotation. These applications are typically more time intensive but may have fewer applicants.
The general consensus recommendation from CORD ASC-EM’s EM applying guide is to apply to 3 rotations per month you are hoping to rotate. Once you have arranged your visiting rotations, please be polite to your fellow applicants and withdraw any outstanding applications from other programs.
For more information on away rotations, see also:
EMRA’s Advising Resources-Finding Away Rotations
ALiEM EM Match Advice Series: VSAS 101 – Securing an away EM rotation
What about the Rest of My Fourth Year?
Beyond their two EM rotations, most students use the rest of their fourth year to complete other requirements for graduation – critical care months, subinternships, or other required rotations. Once you’ve taken care of all of your requirements, consider rotations that are not EM but may teach you skills useful in the ED:
-Critical Care
-Anesthesia
-Ophthalmology
-Orthopedics or Sports Medicine
-Radiology (especially Ultrasound)
-Dermatology
-Neurology, if it’s not part of the core curriculum at your school
Preparing for Your EM Rotation
A comprehensive discussion of how to do well on an EM rotation is beyond the scope of this article. However, as an orphan, you may not be as familiar with EM as students from a program where EM is part of the culture. Here are some resources to help you prepare for and succeed on your rotation:
- CDEM Curriculum is an online textbook of sorts. The “M3 curriculum” covers some of the basic principles of EM. The “M4 curriculum” covers details of disease processes and chief complaints.
- How to get the most out of your rotation
- Reading Recommendations
- Patient Presentations in Emergency Medicine
- Closing the Gap- great resource for laceration repair
- Patient Handoffs (sign-out)
Prior to your first day, make sure to do a little research on the program leadership and glance at the resident webpage to familiarize yourself with the group. Make sure you know: where you are headed, what the parking situation is if you’re driving, whom you are supposed to meet, and BE EARLY! Be friendly to everyone, no exceptions. Ask people their names and try not to forget them. Ask techs or nurses to show you where everything is stocked so you can be helpful in a hurry if the need arises. Most rotations have some sort of “orientation” – pay close attention so that you know what is important.
If you’ve never worked with residents before, this is another aspect of your EM clerkship that might be challenging. It is important to be helpful and inquisitive but also not a burden for the residents you are working with. In the department, scan the trackboard to see who is available to be seen. Always ask the residents on shift if it is okay for you to pick up the patient you are eyeing. Do not skip over or “cherry pick” patients and try figure out who is next up to be seen. Asking is important because there might be a specific reason they do not want you to see that particular patient. For example, the patient might be a “high utilizer” (with lots of visits to the ED) or the resident might want to eyeball them first for stability, etc. Often, you will be paired up with a senior resident and you can ask them if you can practice your presentation with them first.
Presenting
Your case presentations should be brief and focused – often under three minutes. These aren’t inpatient medicine presentations! It is important to include and appropriately emphasize pertinent positives and negatives to show that you have considered all of the “life threatening” items on your differential. As noted above, EMRA has provided some resources about patient presentations. Don’t lie if you are asked a question about your HPI you didn’t collect or part of a physical exam you didn’t do. No one expects you to be perfect. A response of “I don’t know, but I’ll find out,” is the best way to handle when you forget something. Being organized is key to presenting well. Try to present the same way every time. Do not jumble aspects of the HPI, physical exam, review of systems, etc. as it is confusing to whomever is taking your presentation. Even though you may have collected and synthesized the information correctly, it will reflect poorly on you. Don’t feel obligated to present every piece of information you collected. Sometimes, after a few questions, you realize that the item you were asking about isn’t really on your differential, and it’s OK to leave that out from your presentation. If your attending asks about it, you can provide that information then.
At academic medical centers, patients may have long and complex medical backgrounds. Take a few minutes to look over their records. If they have a medical problem you don’t know much about, spend a few minutes looking things up prior to presenting. Check on medication doses that you want to give, review allergies, look up the most likely causes of the disease process you think is going on or what the current treatment recommendations are.
One other common pitfall is forgetting to add a summary and a plan for your patients. The plan should have both diagnostic and therapeutic elements: in addition to checking a lipase because you’re concerned about pancreatitis, propose giving the patient some fluids, antiemetics, and analgesia while you’re waiting for results.
Owning Your Patients
One of the best ways to stand out as a medical student is to absolutely OWN your patients. As a medical student, you are usually expected to carry one patient at a time and know EVERYTHING about that patient. Follow their care from the beginning to the end. If you ordered labs for your patient, circle back in 15-30 minutes to make sure they’ve been sent. If they haven’t, check in with the nurse – maybe even offer to draw them yourself. You might learn that getting an IV on the patient has been difficult, and perhaps you can help out by using ultrasound to get IV access. Has it been several hours since you ordered a CT scan on a patient? Wheel them down yourself. This will make you very popular with nurses and techs and show your dedication to owning your patients. You should be the first to know when labs have resulted or images are able to be viewed. Reassess your patients frequently – ask how they are feeling after pain medications (and order more, if needed) and keep them updated on delays and results. Residents and attendings are very busy and you being a liaison between them and patients will improve patient care and make you look like a rockstar. When you have something to report, be mindful of the workflow of others – best not to interrupt an attending in the middle of running a code to report that your patient’s CBC was normal.
Perhaps the most important thing to keep in mind is that your rotation is a “month long interview.” Your professionalism, interpersonal interactions, and communication skills are being looked at in addition to your clinical skills and medical knowledge. Everyone you come into contact with may have some input about how you might fit in at their program – including not only faculty members but also fellow students, residents, nurses, and other staff members such as the clerkship and program coordinators.
Applying
Although the majority of the application process for an orphan applicant will be the same as for any other applicant, certain parts may be more difficult, and not having someone immediately available to help guide you through the process adds a level of difficulty not faced by other applicants. To start, review the general advice on the basics of the application from CORD ASC-EM in the 2018 Emergency Medicine Applying Guide. You will complete all the same components of the application and have all the same application deadlines. What may be most difficult for you is writing your personal statement and completing your Standardized Video Interview (SVI).
Even though most program directors report that the personal statement is the least important component of the application, you may want to spend more time on this than the average applicant. The personal statement offers a great opportunity for you to address any concerns or weakness your application may have — including being from a school without an EM program. It is better to address any concerns early than wait and hope for the chance to explain them should you be offered an interview. A good way to address a possible perceived lack of understanding of EM may be to discuss how you gained valuable experience from your away rotations or how you found a mentor in EM. You may not need to use your entire personal statement for this purpose but it is wise to include at least a few lines regarding the topic. Ideally, have an EM faculty member review your personal statement – yet another reason to have a mentor to help. There are certain verbiage and language preferred in EM compared to other specialties. You want to give yourself the best chance to match so don’t write off this part of the application. Make sure you budget plenty of time to work on your personal statement when you are planning your fourth year (and then make sure you put that time to good use!)
For tips on writing your personal statement, see page 8 of the 2018 advising guide.
Standardized Video Interview (SVI)
The other part of the application that is different for EM applicants is the Standardized Video Interview (SVI – See p.9 of the 2018 CORD ASC-EM EM Applying Guide for a brief overview.) This new component of the application was piloted in the 2017 Match and is currently specific to EM. As a result, non-EM faculty may have little to no information about or familiarity with the SVI. Since this is a new addition to the application and it continues to evolve, make sure to review the most updated AAMC guidelines prior to completing your interview. At present, the interview must be completed between June 7 and July 15.
Since you may not have a faculty member to help you prepare for the interview you need to use all the AAMC online resources available (AAMC SVI Information & Resources), and do an online practice interview session to help prepare yourself. Data from last year demonstrated a 1 point improvement (out of 25 points) for applicants who prepared for the interview compared to applicants who did not prepare. Even though it is not well understood how programs use this data, it was shown that applicants who did not perform as well on the SVI were less likely to get an interview (CORD SVI Updates). Therefore, this is not an area for you to skimp on preparation. The SVI also serves as another opportunity to demonstrate that you are a great applicant deserving of an interview.
Interviews
Interview season is an exciting but also stressful time for applicants. As a student without a home EM residency program, you will have to take more initiative in collecting information about how to choose the programs you apply to and interview at. Again, having a mentor who is knowledgeable about the applying process, who has gotten to know you before interview season starts, can be invaluable in making the difficult decision between two programs. The program and clerkship directors at your away rotations, or any residents that you feel comfortable speaking with are other resources to consider. The resources listed at the bottom of this document can also help provide some information about programs.
For general advice for interviews, refer to the CORD ASC-EM Emergency Medicine Applying Guide.
Choosing your interviews
How many interviews you need to go on will depend on your application and your preferences for location and type of program. Many people will first pick programs by location, and then go from there. If you find you are in the fortunate position of having too many or conflicting interviews, you may need to cancel interviews or pick between programs. According to the 2018 NRMP Charting the Outcomes in the Match, the probability of matching reaches 99% at about 13-14 contiguous ranks for US Allopathic and Osteopathic seniors. This means after about 13 interviews, you are not really increasing your chances of matching. See this post from The Vocal Cord for a short but relevant read about the number of interviews to attend.
Pre-match communication
After each interview, it is always a good idea to write thank you notes or emails to the program / people who interviewed you. Most programs will be happy to answer any questions you have throughout the rest of interview season. “Second looks” are opportunities to come back to a program a second time, outside of your interview day, to revisit a program, talk to more residents, perhaps see more of a town. These are sometimes offered by programs but are by no means required or necessary. You should only spend time/money on a second look if you feel it will benefit your decision making, NOT to show interest in the program. If you visit various student blogs, you may see some students who suggest sending letters telling programs that you will rank them favorably (this trend was known as sending a “letter of intent” a few years ago, akin to how college athletes are recruited.) “Love letters” to programs are fine, as long as they are genuine. Do not tell more than one program they are at the top of your list – EM is a small community, and word gets around quickly. On the flip side, you may be contacted by a program telling you that they are ranking you highly. There is no way to know if this is true or not, and the general advice is to not let such communications affect your rank list. The Match algorithm favors the applicant, and there is no “bonus” for matching at a program that has also ranked you highly.
Making your Rank List
Making your rank list is personal and the experience will be different for everyone. Page 13 of the 2018 Emergency Medicine Applying Guide has a great summary of different factors and strategies that some students will use to rank programs. As stated before, it is really important to have found a mentor by this point that you feel comfortable discussing your rank list with if you do need help. Other medical students can be good resources to share ideas and opinions with, but be cognisant that a program one student disliked may be perfect for another, depending on what each student feels is important to them. Although ranking your programs will undoubtedly be stressful, take solace in the fact that the majority of medical students will match to one of their top three choices.
Summary / Key Points
Regardless of where you are in the process (first year student or final year student), find an adviser early who is familiar with the EM application process to discuss your application, help gauge your competitiveness, and come up with a back-up plan if needed.
- Competitive USMLE Step 1 and Step 2 scores will enhance your chances of matching into an Emergency Medicine Residency Program. A USMLE Step 1 score <220 warrants taking Step 2 CK early as well as considering a back-up plan.
- Try to complete two audition elective rotations at ACGME residency-based training programs before October of your fourth year.
- Aim to get 2 Standard Letter of Evaluations (SLOEs) from ACGME EM programs submitted as early as possible, with at least one uploaded by the time ERAS opens on September 15th.
- Prepare for your rotations, work hard, and do well on your “month long interview.”
For additional resources on ALL of the above topics (and much, much more) check out the ASC-EM Curation of Existing Resources list and the ASC-EM website.
References:
National Resident Matching Program, Charting Outcomes in the Match for U.S. Allopathic Seniors, 2018. National Resident Matching Program, Washington, DC. 2018.

[…] Orphan Applicant Emergency Medicine Applying Guide […]
LikeLike