Authors: Liza Smith MD, Emily Hillman MD, Elizabeth Karr, DO, Ross Christensen MS4, Megan Stobart-Gallagher, DO, Lucienne Lutfy-Clayton MD and Adam Kellogg MD on behalf of the CORD Student Advising Task Force
The CORD Student Advising Task Force created the Emergency Medicine Applying Guide as a comprehensive guide to help applicants and their advisors navigate the entire Emergnecy Medicine match process. The Applying Guide is targeted at the average EM applicant. This post is a supplement to that document with recommendations specific to the Osteopath trained applicant. Please pass this along to your student advisees and anyone else you think it would help.
Background: Historically, there have been two paths for the osteopathic student (DO) pursuing Emergency Medicine (EM)—applying to osteopathic-affiliated residency programs under the American Osteopathic Association (AOA) match or to allopathic residency programs under the Accreditation Council for Graduate Medical Education (ACGME) match, otherwise known as the National Resident Matching Program (NRMP).
In February 2014, the ACGME, AOA, and American Association of Colleges of Osteopathic Medicine (AACOM) announced a path towards formation of a single graduate medical education accreditation system. Under this plan, AOA-approved programs can apply for ACGME accreditation by June 2020, when the AOA will cease all primary accreditation activities and all EM training programs will be under the ACGME umbrella.
What about existing AOA-approved programs?
Starting with the upcoming match season (2017 – 2018), many osteopathic programs will have already converted to their initial ACGME accreditation. Many of these “traditional” AOA-approved programs will also be pursuing an additional “Osteopathic Recognition” in which programs plan to pursue an osteopathic-focused learning environment. This may include, but not be limited to, integrated Osteopathic Principles into clinical rounds, dedicated Osteopathic Manipulation conference, and focused rotations focusing on core Osteopathic principles. Allopathic graduates will be accepted into these programs, but there will be some pre-matriculation requirements, yet to be determined. More information regarding “Osteopathic Recognition” and its requirements for programs can be found on the ACGME website.
This applying guide is intended for the osteopathic applicant seeking to pursue a successful match in the ACGME system.
Why do osteopathic students want to apply to allopathic (ACGME) programs?
The reasons often given by rotating students and residents who went to osteopathic schools:
- The opportunity to train in larger medical centers
- Option for three-year training programs
- Academic affiliations of the training programs
- Larger sized programs and the stability that comes with them
- Greater perceived opportunities for fellowships and jobs
- More programs to choose from
- Avoid uncertainty with the planned AOA merger
- Opportunities to obtain EM board certification with either ABEM or AOBEM.
What are the obstacles in applying?
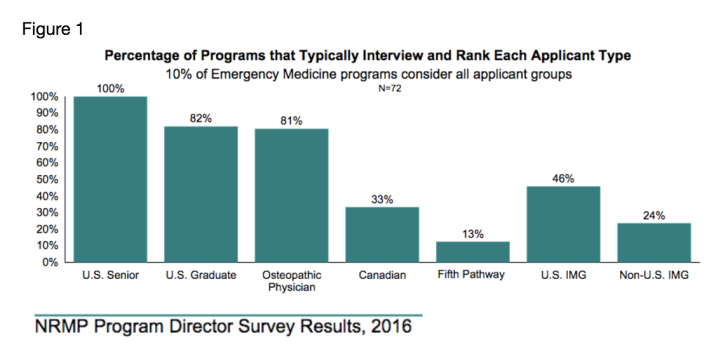
The biggest obstacle to an osteopathic student’s application to the ACGME system is perceived competitiveness. The issue of bias against DO students in the selection process is very real. Only 81% of traditionally allopathic programs will typically interview and rank DO students (Figure 1)1, narrowing the number of programs available to apply to overall. There is no ‘official list’ of programs who are or are not welcoming of DO applicants, so it will take some legwork in order to best create your application list.
One common strategy is to look at the composition of the current residency classes at an institution—if they have DOs, especially if they have matched someone from your school, they will likely consider your application. If they have no DOs, you are unlikely to be the first.
Another way to find programs welcoming to DOs is by using EMRA Match, a searchable on-line EM residency database. Residency programs can be sorted by the percentage of DO residents in training there. Just because a program has few or no DOs does not mean they are definitely closed to their applications.
Some programs who give consideration to both types of students will rank academically equal MDs above DOs. Not surprisingly, to be successful in matching you need to stand out as a candidate and be strategic in planning your application.
To put things in perspective, in the 2016 match, of the 290 osteopathic students who applied to emergency medicine, only 76% of those matched.2 To ensure your ability to match, it is imperative to have a strong application.
What can I do to maximize my chances?
Before fourth year
First, it’s important to avoid any “red flags” on your application that would diminish your chances of matching. These include failing classes, failing or scoring low on COMLEX or USMLE boards, felonies, and professionalism issues.
Second, get involved with EM-related organizations. Be active in your school’s EMIG, join EMRA, SAEM, or other professional organizations.
Third, find a mentor who is involved with an ACGME residency. These people are the most familiar with the application process and will be able to give the highest quality advice. They can give you feedback on your application and help you figure out how many places to apply as well as guidance as to where to apply. A good mentor, especially if your school isn’t affiliated with a training program or if it lacks EM faculty for advisement, can be critical. How do you find a mentor? Go to regional or national conferences. Ask upperclassmen if they know anyone. Reach out to a program you’re really interested in. Faculty mentors are often available during your out-of-town rotations; consider asking one of their residency leaders for advising.
Maximizing Your Application
To even the playing field, you need to make yourself as competitive as possible to allow programs to compare you apples-to-apples with your allopathic peers. The three areas where this is most critical are your board scores, your EM rotation grades, and your Letters of Recommendation.
Board Scores:
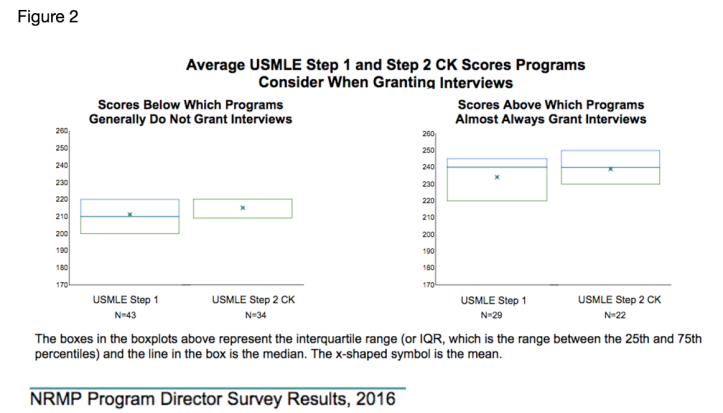
First, you MUST take the USMLE Step 1 AND Step 2 CK if at all possible. If you are only able to take Step 1 that is much better than taking neither. Failure to take at least one will hinder your application. These tests allow your knowledge base to be compared directly to your MD peers. USMLE scores around 235 or greater will help you get interviews. Scores less than 220 may make it much more difficult for you to get interviews (Figure 2)1. If possible, try to take Step 2 early in 4th year so that you can have your scores released by October 1st, especially if your Step 1 score is <220.
For context, the average COMLEX scores of DOs who match into allopathic EM programs are 593 and 610, for level 1 and level 2 respectively.2 Keep in mind that many allopathic residency directors will be unwilling to translate a COMLEX score to an equivalent USMLE score, or will look for a grossly higher COMLEX score than the equivalent USMLE score.
Rotations:
You will need to try to secure at least two EM audition electives, at least one of which should be at an ACGME residency. You will want to complete two EM clerkships as early as possible in your fourth year, ideally before mid-September, in order to have your Standard Letter of Evaluations (SLOEs) available when the Electronic Residency Application Service (ERAS) opens on September 15th. You will be side by side with your allopathic peers on these rotations and will demonstrate your performance in an academic setting similar to the residencies to which you will be applying.
Note that many academic programs use the Visiting Student Application Service (VSAS) for audition rotations, which often opens to accepting applications in early March. Keep your eye out for any program-specific application requirements! For example, programs may require a brief personal statement or even favor students originally from the area. Programs will use audition rotations as a recruitment tool as much as you do!
Letters of Recommendation:
The letters of recommendation that carry the most weight are going to be in the SLOE (Standardized Letter of Evaluation) format and come from residency program leadership. You should aim to get two SLOEs from academic residencies, preferably group SLOEs written by the educational teams where you rotate. These letters carry more weight than the traditional letters of recommendation because they provide context for direct comparison of you to your EM-bound peers by people integral to the EM match process. These standard letters are one of the most frequent omissions from osteopathic applications, making it difficult to accurately compare them to the rest of the applicant pool.
While community EM months can be great learning experiences and expose you to how the majority of EM physicians practice, they will not significantly assist your application to an allopathic EM residency. A letter of recommendation, or even a SLOE written by a doctor at a community ED is not the same thing as one from an ACGME program and should not be counted as equivalents. If your school requires a community EM experience, you will have to do extra clerkships in EM, and in some instances, even forgo credit to gain opportunity and advancement in your application.
What are your chances?
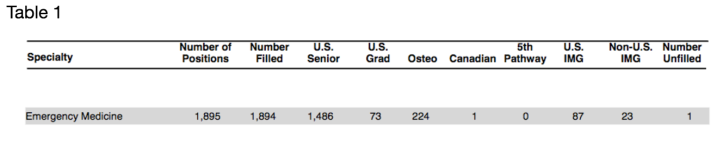
Approximately 12% of ACGME EM slots go to Osteopaths (Table 1)3, so you have a chance, but you need to be smart about your application. A successful match will require planning in order to have taken the USMLE and have 2 audition electives scheduled early in your fourth year, preferably before October. It will depend on strong clerkship grades and supportive SLOEs submitted to ERAS as early as possible. It will require some research to make sure the programs you apply to are open to interviewing and matching osteopathic applicants.
How Many Programs should I apply to?
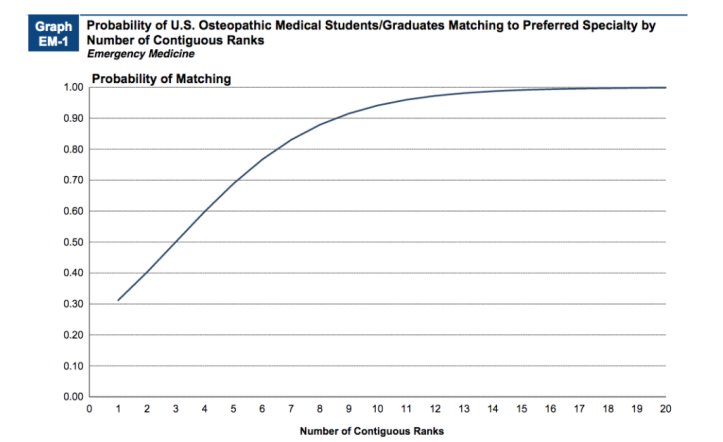
Data show that applicants who ranked 9 programs had a ~90% match rate in EM. Those with 12 or more programs pushed that match rate up to 95-99% (Figure 3)2. Depending on the strength of your overall application (USMLE scores, EM clerkship performance, SLOEs, etc), you should consider applying to somewhere between 30-40 realistic programs in order to obtain 12 interviews and have a good chance of a successful match.
Do not limit yourself in the programs you apply to. If there is a program that is high on your list, but does not commonly accept DOs, you should still apply to it. However, you may not want to count this in the overall number of places you are applying to. In other words, apply to 30-40 programs which you think you have a high likelihood of getting into and which commonly accept DO students. Once again, reach out to an advisor if you are unsure about your competitiveness, if you think there might be red flags in your application, or board scores that make you less competitive.
This numbers question truly requires an individualized answer from an advisor familiar with the EM application process who can help you assess how competitive an applicant you are. For a less competitive applicant it is important to have a frank discussion about a back-up plan in case the interviews are not forthcoming.
What are some tools and resources that can help me?
There are a lot of great resources out there. Here are a few of the high-quality ones:
Should I worry about board certification?
In short, not right now. However, it might be something to think about when considering a program with Osteopathic Recognition – which may expect you to become AOBEM certified.
Currently, osteopathic graduates of AOA-accredited residency programs are required to take the AOBEM board certification and must maintain membership in the AOA in order to maintain certification.
Osteopathic graduates of ACGME residency programs can become either AOBEM or ABEM board certified in EM. Once again, even if you graduate from an ACGME program and choose AOBEM certification, you must maintain membership within AOA. Both certifications require recertification testing and continuing medical education (CME) requirements. These can be found in more detail on their respective websites.
Summary points
- Take the USMLE Step 1 and Step 2 to allow your knowledge base to be compared apples to apples with your allopathic peers. A USMLE Step 1 score <220 warrants taking Step 2 CK early as well as considering a back-up plan.
- Try to complete two audition electives at allopathic residency-based training programs before October of your fourth year.
- Aim to get 2 Standard Letter of Evaluations (SLOEs) submitted as early as possible, ideally before ERAS opens on September 15th. These SLOEs need to be from ACGME EM programs.
- Be strategic with your application: do some legwork to identify programs that are open to interviewing and matching osteopathic candidates.
- Find an advisor familiar with the EM application process to discuss your application, help gauge your competitiveness, and come up with a back-up plan if needed.
References
-
National Resident Matching Program, Data Release and Research Committee: Results of the 2016 NRMP Program Director Survey. National Resident Matching Program, Washington, DC. 2016.
-
National Resident Matching Program, Charting Outcomes in the Match for U.S. Osteopathic Medical Students and Graduates, 2016. National Resident Matching Program, Washington, DC 2016.
-
National Resident Matching Program, Results and Data: 2016 Main Residency Match®. National Resident Matching Program, Washington, DC. 2016.

This is good straight forward info. Thanks for your work!
I want to point out though, the Probability graph assumes that these contiguous ranks are random and interviews are certainly not random! I believe there’s much more value to studying Chart EM-2 the Number of contiguous ranks (page 36). This shows that in 2016 even students with just 5 interviews had a much higher rate of matching. And students with just 8 interviews matched at 20 to 1!
I’ve been making a plea to downplay the probability graph for a long time, since “red-flags” and performance during an interview are huge factors. Just ask the person who had 14 interviews and didn’t match!
LikeLiked by 1 person
Thank you for this post which will be helpful to those participating in this new single GME accreditation system. Here are a few facts from the American Osteopathic Association (AOA) to further strengthen the piece.
First, the word “osteopath” refers to a health professional outside the US that uses osteopathic manipulative medical techniques. Osteopaths often are are physical therapists. In contrast, osteopathic physicians are individuals who have completed four years of education in a US college of osteopathic medicine. American dictionaries are currently revising their definitions to clarify this point.
Second, we are embarking on a new, single GME accreditation system; it is not a merger. This transition includes a change in the governance at the ACGME, additional DO members of the board and review committees, and a new SVP of osteopathic accreditation. The reasons for a single accreditation system include consistent methods of evaluation and accountability; enhanced opportunities for all trainees; and one accreditation system transparent to the federal government, licensing boards, credentials committees, the public, and others.
Third, you indicate that students must take the USMLE examinations. This is the current process for ACGME EM programs, but is not the process for AOA EM programs transitioning into the new system. It is expected that program directors that accepted COMLEX before will continue to use COMLEX scores. Moreover, around 77% of allopathic program directors will accept COMLEX scores; we hope that EM program directors are part of that group. Many program directors agree that it is the “fit” of the student in the residency program that is the single most important issue to a program director. COMLEX and USMLE examinations are not intended to be used as a criterion for entry into residency training.
Regarding certification, the AOA expects that physicians who take an osteopathically recognized training position will want to take an osteopathic board certification examination as the most appropriate indicator of their expertise. However, every graduate of an ACGME program has the option of sitting for the ABMS board, even if they participated in an osteopathically-recognized position.
Lastly, the post discusses the requirement that osteopathically certified physicians must be members of the AOA. The AOA is actively working to revise this requirement.
LikeLiked by 1 person
[…] Emergency Medicine Applying Guide. Council of Residency Directors Blog. 2017. Available at: https://cordemblog.wordpress.com/2017/02/02/the-osteopathic-emergency-medicine-applying-guide/. Accessed May 28, […]
LikeLike